Improving wound care and preventing infection
Research carried out by the Skin Interface Sciences research group (a collaboration between the Schools of Applied Sciences, Human and Health Sciences, Computing and Engineering and Art, Design and Architecture), has helped to shape policy and practice in the field of surgical site infection (SSI) and wound management.
What was the problem?
Over 5 per cent of patients in the UK undergoing surgery acquire an SSI, and three quarters of the deaths following SSIs are due to this infection. SSIs account for around 15-20 per cent of all healthcare-associated infections, leading to increased morbidity and mortality, additional costs and longer stays in hospital.
Benefits of this research
The group has developed best practice guidance and helped raise practitioner, industry and public awareness of the importance of effective clinical interventions in infection prevention, tissue viability and wound care. The Skin Interface Sciences research group has helped to address these concerns by promoting effective clinical care in tissue viability and wound care. Much of this work has focused on how wound complication rates, post-operative surgical blisters and the healing and infection of chronic wounds are affected by the choice of dressing.
What did we do?
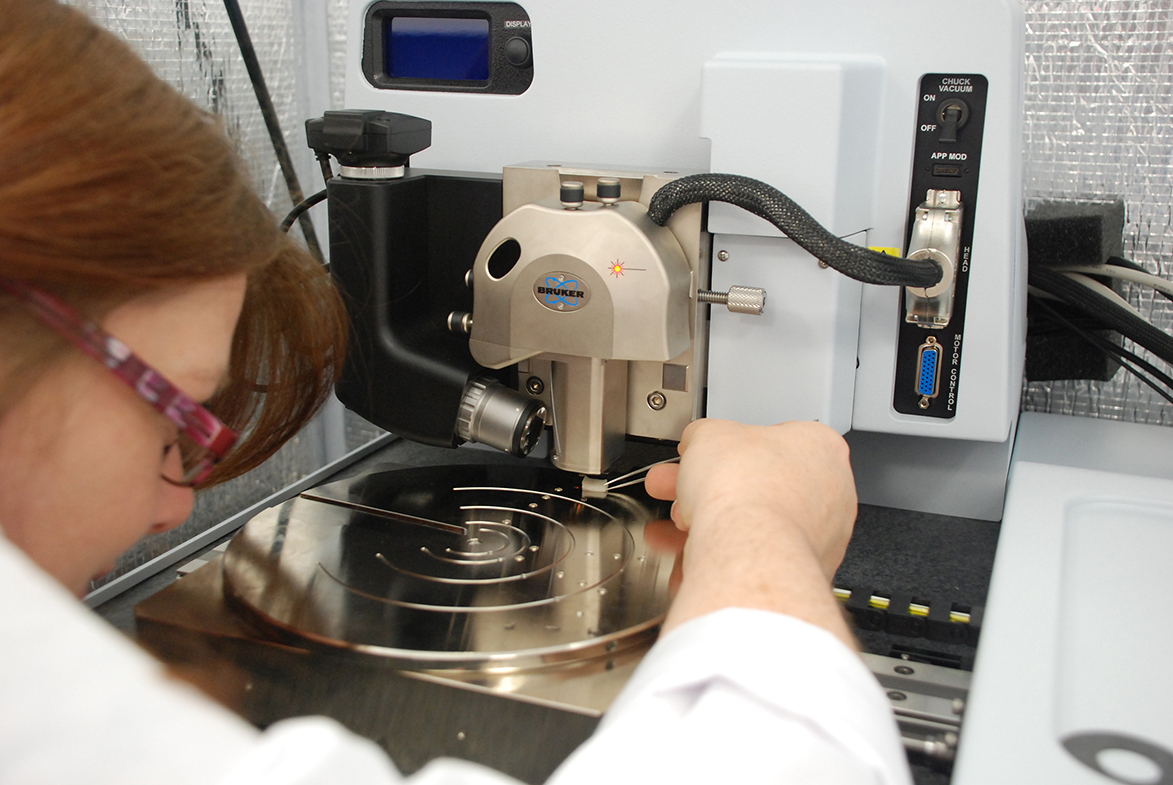
Antiseptics can contribute to SSIs as they often exhibit restricted penetration into the skin, limiting their efficacy against microorganisms when the protective skin barrier is breached during surgery. A collaboration between the University of Huddersfield, University Hospital Birmingham and Aston University investigated the factors controlling the release and effectiveness of the antiseptic, chlorhexidine gluconate (CHG), released from a drug-impregnated gel dressing. The study revealed that the CHG gel dressing could maintain antimicrobial activity for up to seven days, potentially suppressing bacterial growth and helping to prevent infection.
The team at Huddersfield has conducted an on-line survey of international experts producing best practice guidance for the prevention of surgical wound blistering. Based on contributions from respondents in Scandinavia, India, Australia and the US, the consensus emerged that an ideal wound dressing should easily conform to the wound, allow for swelling and have simple application and removal, thus minimising pain for the patient.
An e-learning resource, Challenges in Wound Care, has also helped to develop and support best practice in this area by drawing on the research group’s experience. Using a problem-based structure to address questions surrounding the assessment, diagnosis and management of various wound care scenarios, it promotes the importance of working in a multidisciplinary team to achieve optimum outcomes for patients.
These projects have helped to shape policy and practice in areas including planning interventions, quality of life and well-being – which are vital if patients are to receive evidence-based, cost-effective treatment. This work has contributed to a series of influential Best Practice Statements, including The Use of Topical Antiseptic/Antimicrobial Agents in Wound Management. This publication is widely used as evidence to support NHS Trust development and to guide the use of appropriate dressings for the management of wound infection.
What happened next?
Dr Karen Ousey has led much of Huddersfield’s work in this field as a key member of the Skin Interface Sciences research group. Her research into reducing the risk of surgical site infection (SSI) in cancer patients after spinal surgery won first prize in the Hard-to-Heal Wounds category of the 2012 Wounds UK Awards, and she was also highly commended in the Patient Experience category of the 2013 Journal of Wound Care Awards. In early 2014 Karen was awarded a scholarship from the Florence Nightingale Foundation to carry out collaborative research into improving the quality of life for those suffering from serious wounds.